When people think of eating disorders, they often picture young individuals engaging in ritualistic food consumption and worrying about their food choices, portions, ease of digestion, and appearance due to bloating. Others perceive people who have eating disorders as being quite similar to people who have body dysmorphic disorder in that they are both fixated on their appearance. However, most individuals do not consider eating disorders to be on the same spectrum as OCD, and the connection between the two diseases has undergone relatively little research. Even more concerning is that doctors typically confuse one for the other when patients seek the assistance of mental health specialists to relieve their distress. To put it another way, it may be challenging to distinguish between OCD and eating disorders in patients who have both at the same time. If so, which condition is mostly to blame for the other, given how similar their resulting behaviors may seem?
Learn more about the link between OCD & Body Dysmorphic Disorder.
A Quick Guide
It’s not rare to have another mental health condition in addition to having an eating disorder like anorexia, bulimia, or binge-eating disorder. Depression, generalized anxiety disorder, social anxiety disorder, post traumatic stress disorder, and obsessive-compulsive disorder are a few of the conditions that may be present.
In actuality, research indicates that around two-thirds of individuals with eating disorders also have an anxiety disorder. The most prevalent of them is obsessive-compulsive disorder (OCD). Indeed, research has found that individuals with eating disorders like anorexia nervosa or bulimia nervosa are anywhere between 11 and 69% more likely to experience OCD. It is thought that eating disorders and anxiety disorders have characteristics in common that help to shape them and explain the high occurrence of comorbidity.
What is Obsessive Compulsive Disorder?
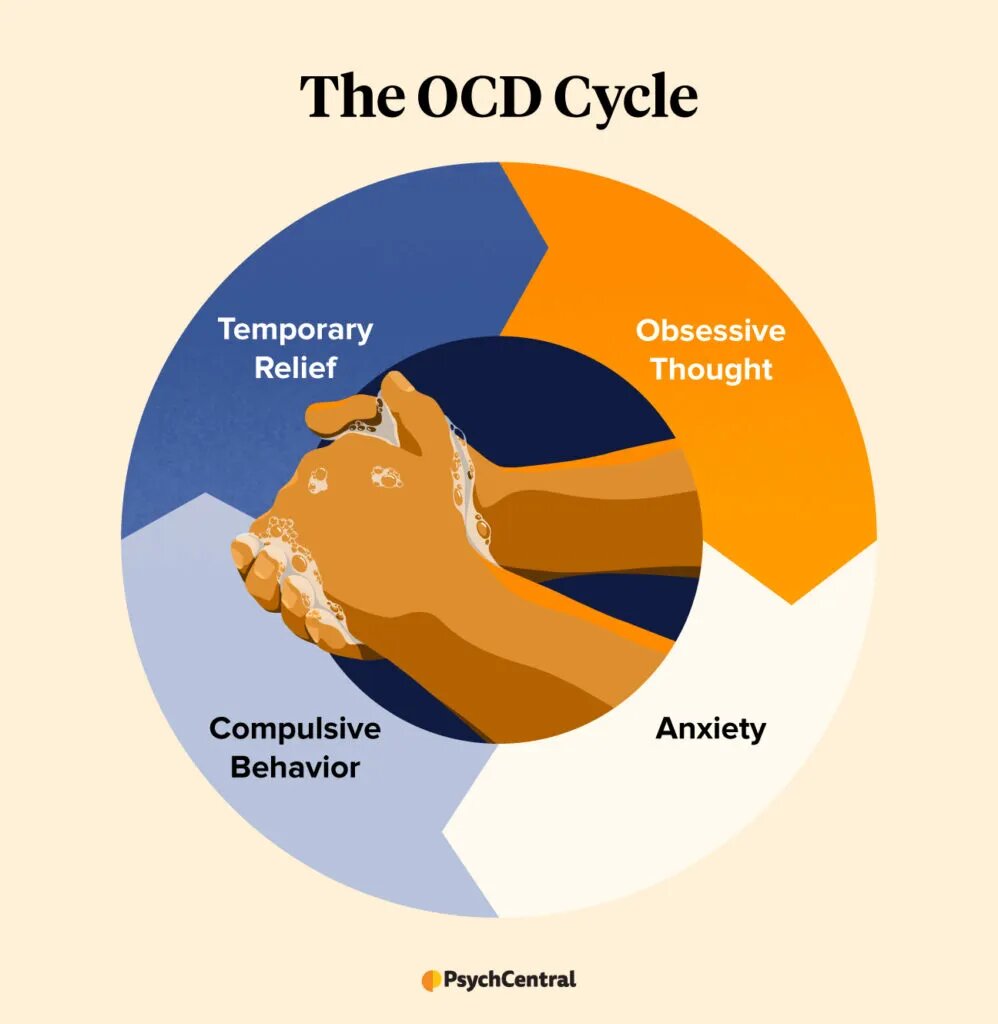
When an individual experiences persistent and ongoing obsessions and compulsions, they are diagnosed with OCD.
Persistent, uncontrollable thinking is an obsession. When someone has OCD, they will repeatedly engage in various actions to combat their fixation. These actions are referred to as compulsions. For instance, somebody might have a severe phobia of germs. They could overwash their hands as a coping mechanism for this phobia.
Common Symptoms
Someone with OCD experiences a cycle of obsessions and compulsions, as was already explained. Obsessions are a typical trait among OCD patients. These consist of:
- Fear of contamination or pathogens.
- Thoughts that are prohibited or disturbing regarding violence, religion, or sex.
- Aggressive thoughts, either toward oneself or others.
- Needing everything to be precisely symmetrical or arranged.
Common compulsive behaviors include:
- Extreme washing of hands or cleansing.
- Needing to arrange things in a specific manner.
- Checking on things repeatedly.
- Continually making sure the door is locked.
- Obsession with counting.
While OCD’s two primary symptoms are compulsions and obsessions. There are several other symptoms. These include:
- Having no ability to control one’s thoughts or actions, especially when they are severe.
- A person spends more than an hour of the day engaged in these thoughts or actions.
- Although rituals and behaviors are unpleasant, they offer momentary relief from intrusive thoughts.
- Because of these attitudes and behaviors, they have a significant impairment in their capacity to function at work, in school, in relationships, or even performing simple chores.
- Avoiding circumstances that make their obsessions worse. For instance, a person with a phobia of germs might refrain from going outside.
What Leads to OCD?
It’s difficult to pinpoint the precise factor that contributes to OCD in each individual. This is due to the unique genetic makeup and life experiences of every individual. OCD may have various causes, including:
Genetics: According to research, those who have an OCD parent, sibling, or kid are more likely to develop the disorder themselves.
Brain anatomy and function: Some OCD patients have altered neural connections. What causes these alterations is still a mystery to researchers.
Environment: Childhood trauma is linked to OCD. Additionally, childhood bacterial illnesses like streptococcal infection have been related to OCD.
Can an eating disorder result from OCD?
Researchers are unsure of the unique factor that triggers an eating disorder. OCD symptoms are more likely to resemble those of eating disorders. Despite the frequent co-occurrence of OCD and eating disorders, nothing is known about this.
Because it can be challenging to distinguish between these two illnesses, medical practitioners must thoroughly evaluate each patient’s case to determine the exact cause of their symptoms. We should understand more about the connection between OCD and disordered eating as more research examines this association.
Relation between OCD & Eating Disorders
OCD patients and those with eating disorders both experience intrusive thoughts and compulsive behaviors. However, these obsessions and compulsions are often restricted to ideas and behaviors regarding food and/or weight in persons who simply have an eating disorder. For instance, they might overdo exercise or constantly count calories. A person with an eating disorder may also be suffering OCD symptoms if they also have obsessions and compulsions concerning other aspects of their lives. It’s interesting to note that a 2003 study indicated women who had OCD as children had a higher risk of later having an eating disorder.
It’s possible for people with eating disorders to exhibit symptoms that are strikingly similar to OCD symptoms. For instance, those who struggle with eating disorders may have frequent worries about their diet, weight, and appearance. They might also practice ritualistic habits like routine weighing and bodily checks.
People with eating disorders do not consider these ideas and behaviors to be troublesome, whereas people with OCD often regard these thoughts and behaviors to be upsetting or unpleasant. When a person has an eating disorder, their attitudes and actions support the disorder and help to maintain it.
Watch: [What is compulsive Eating Disorder?]
AFRID and OCD
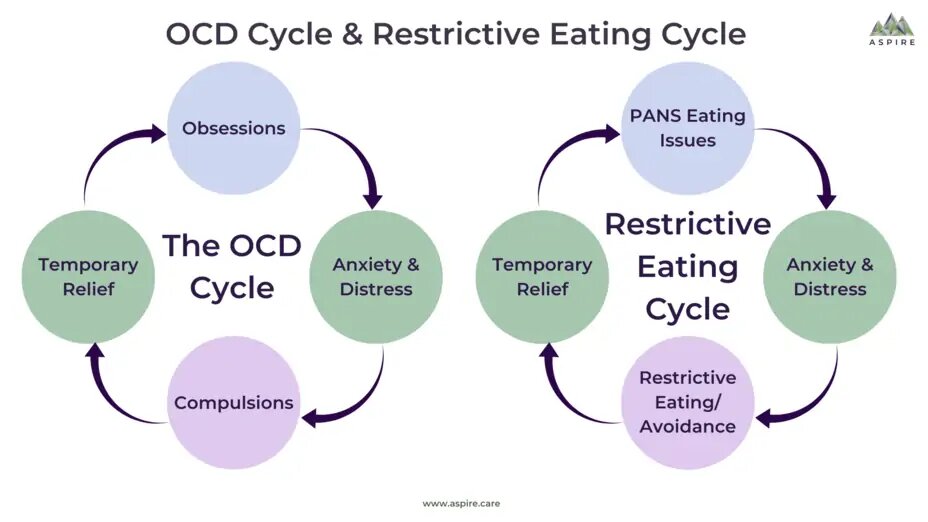
We frequently observe an overlap between OCD behaviors and symptoms and the eating disorder diagnosis of ARFID (Avoidant Restrictive Food Intake Disorder). People who struggle with ARFID have acute sensitivities to eating as well as a severe lack of interest in or aversion to food. They could feel heightened or distorted in relation to tastes, textures, or smells. They frequently quit eating a certain meal because of unpleasant past interactions with it or the eating process. While many eating disorders (including sub-clinical disordered eating) exhibit obsessive and compulsive thoughts and behaviors, ARFID is an illness with a specific concentration of overlapping symptoms.
Orthorexia and OCD
Orthorexia is not a recognized eating disorder in the medical community. However, specialists in eating disorders are now aware of a persistent pattern of unhealthy, obsessively healthy eating.

Because they are drastically limiting the kinds of food they eat or banning particular food groups, people with orthorexia frequently become malnourished. A person with orthorexia might eliminate all carbohydrates or sugars, for instance. People with OCD and orthorexia may adopt specific rituals related to food in an effort to control their anxiety.
Binge Eating Disorder and OCD
It may be challenging to distinguish between OCD and binge eating disorder (BED). BED is not the same as OCD, other than sharing some compulsive characteristics. People who have BED overeat compulsively and find it difficult to control their behavior. Binge eating can occur as a result of stress, but it is possible for someone to both have OCD and BED.
Anorexia and OCD
When someone has anorexia, they will exhibit the following symptoms:
- Body mass index that is abnormally low or difficult to keep a healthy weight.
- Extreme anxiety about putting on weight or getting fat.
- Lack of awareness of the seriousness of their issue.
- Their bodily form or weight has a significant impact on their sense of self.
People with OCD and anorexia may experience obsessive thoughts about food or weight and, as a result, may engage in ritualized eating to help them cope with their anxiety about food. For instance, they might need to ensure that their plate is exactly symmetrical.
How is it differentiated?
It is essential for the doctor to carefully investigate the precise behaviors that are being seen and the motivations behind those behaviors in order to differentiate between the two diseases and make the correct diagnosis. Patients with eating disorders, however, adjust their eating habits to lose weight in accordance with their concerns about their physical appearance. Patients with OCD may limit their meals for reasons unrelated to worries about their appearance. Additionally, in situations where a person meets the criteria for both diagnoses, such as when a bulimic or anorexic person also exhibits non-food-related OCD symptoms, such as contamination or checking, it is crucial to think about whether or not their symptoms are being driven by both disorders at once. Consider a patient who washes their groceries out of concern for contamination and the possibility that the items contain high-fat contents.
Treatment options
When a person has symptoms of multiple conditions, it might make therapy more difficult. Fortunately, both eating disorders and OCD can be effectively treated. The most common treatments for obsessive-compulsive disorder are medication and/or psychotherapy.
Medication
There are certain drugs that have been proven to be effective for OCD. These drugs are classified as selective serotonin reuptake inhibitors (SSRIs). Antipsychotics are additional drugs that have been demonstrated to be beneficial.
Therapy
OCD is known to respond well to some types of therapy, including Cognitive Behavioral Therapy (CBT). One CBT strategy, in particular, is applied to OCD. The name of this method is Exposure Response Prevention (ERP). ERP involves subjecting a person to an obsession-triggering stimulus. ERP sessions would make the person who has a germ phobia dirty their hands and then restrict them from indulging in their obsession.
It’s critical to understand that ERP increasingly intensifies with time. ERP is a process that develops into the most stressful condition as a person shows they can handle it. OCD has been demonstrated to respond well to ERP.
Relapse Prevention and Aftercare Support
There are certain relapse prevention strategies that may be beneficial for people with eating disorders and OCD that co-occur. Which are:
- Preparing for the future. Find out what your triggers are and prepare yourself with appropriate coping mechanisms.
- Visit a counselor. After symptoms have settled, some therapists will meet with clients every two weeks or once a month. Having a therapist at your side can be beneficial for maintaining your development and enhancing your resilience.
- Attending OCD or eating disorder support groups.
- Using mindfulness techniques.
- Keeping your support system informed.
- Maintaining a regular medication schedule.
- Limiting your social media usage to as many body-positive accounts as you can.
- Using relaxation or stress-reduction methods.
- Thinking back on relapses. Find out what caused the lapse and how to handle a situation similar in the future by speaking with a therapist.
Family Counseling
Family counseling is occasionally a part of family support. Having a family approach combined with other treatments helps patients’ recovery and rehabilitation.
We hope you found this article useful in learning more about how OCD can relate to eating disorders. Do You Get Anxiety After Eating Carbs? Here’s How To Manage



 Healing Your Inner Child: A Short Guide
Healing Your Inner Child: A Short Guide  What You Need to Know About Trauma & its effects
What You Need to Know About Trauma & its effects  Dealing with a Narcissistic Parent: Strategies and Support
Dealing with a Narcissistic Parent: Strategies and Support  Understanding the MBTI Personality Types
Understanding the MBTI Personality Types  Understanding the Big Five Personality Traits
Understanding the Big Five Personality Traits  Body Image: what it entails and how it affects you
Body Image: what it entails and how it affects you