A Quick Guide
Autism spectrum disorder ASD is a neurodevelopmental condition characterized by difficulties in social communication, narrow interests, and repetitive behaviors. People with ASD are more likely to develop comorbid psychiatric disorders. In this article, we will discuss the different types of comorbid psychiatric disorders in people with ASD.
Understanding ASD
The main characteristics of Autism Spectrum Disorder that cause dysfunction may also include behavioral and emotional issues. Recent estimates of ASD prevalence in the United States range from 1.68% among people aged 8 in an active public health surveillance program to 2.41% among people aged 3 to 17 based on a national parent survey, with male-to-female ratios of 4.0 in the group of people aged 8 and 2.9 in the group of people aged 3 to 17 years. Compared to those who are ordinarily developed, people with Autism are more prone to develop comorbid psychiatric disorders including depression, anxiety, or bipolar disorder.
Factors behind comorbid psychiatric disorders
The higher likelihood of comorbid psychiatric disorders is caused by a variety of circumstances. Bullying and unfavorable life events are more likely to occur in people with autism, who are also more stressed out and at risk of developing depression and anxiety. ASD’s cognitive rigidity, issues with emotion regulation, and sensitivity to change can put these people at higher risk for depression and anxiety. Deficits in emotional regulation may be a cross-diagnostic phenomenon that underlies anxiety and other psychiatric comorbidities, as well as the characteristics of ASD.
How are comorbid psychiatric disorders assessed?
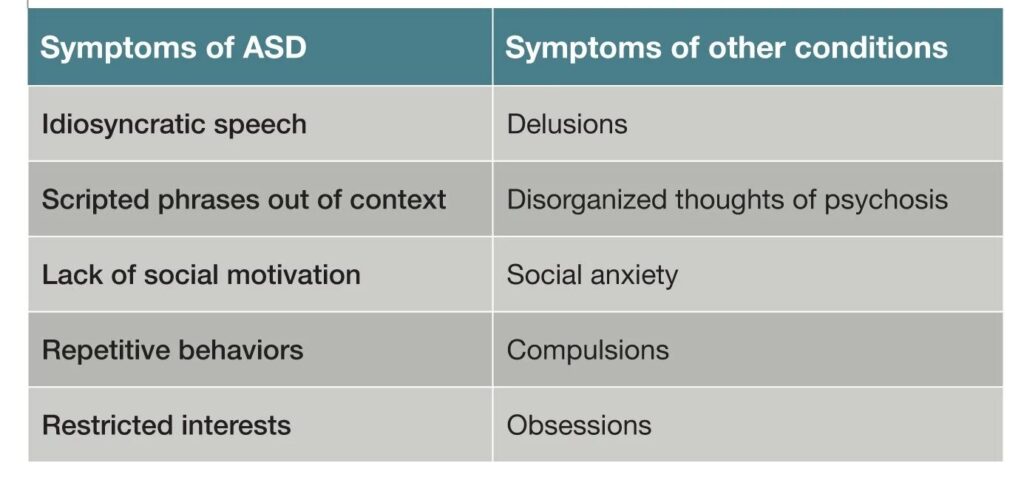
It may be difficult to distinguish the characteristics of ASD using screening tools made for psychiatric illnesses in the general population, which can lead to overdiagnosis. To assess for comorbidities in children and adults with ASD, a number of validated disorder-specific instruments have been created. It can be challenging to discern between symptoms that pertain to the basic features of ASD and symptoms of many other psychiatric disorders since traits of ASD sometimes seem to coincide with symptoms of other conditions.
The following factors are considered:
Create a baseline
It’s crucial to set a person’s baseline for optimal performance. It is vital to identify baseline behaviors and functioning from unique variations in symptoms that are expected with the start of a co-occurring psychiatric disease for episodic psychiatric conditions (eg, mood disorders) or those that come later in development (eg, OCD, psychosis).
Check for any medical co-morbidities
Examine your health for any conditions that can make your emotional and behavioral issues worse, especially if you are a less talkative person.
Consider genetics
Some genetic syndromes have been linked to behavioral traits and psychiatric disorders. This may facilitate more focused screening.
Take developmental level into account when analyzing symptoms
If a person exhibits symptoms that go beyond what would be reasonable given their mental age and developmental stage, comorbid conditions should be taken into consideration.
Comorbid Psychiatric disorders
Let us discuss some common comorbid psychiatric disorders with autism.
Watch: [Psychiatric Comorbidities]
Anxiety disorders
In children and adolescents with ASD, anxiety-related issues are among the most frequent presenting issues in the clinical context. Simonoff et al. discovered that 41.9% of the 112 ASD children they evaluated between the ages of 10 and 14 matched the diagnosis for at least one anxiety condition. The most frequent anxiety disorder was social anxiety (29.2%).
Because those with higher levels of anxiety are more conscious of their own social dysfunction, they have lower IQ scores and less severe ASDs. When compared to peers who were of the same chronological and mental age, ASD children displayed a wide variety of phobias and fears, reporting more frequent medical and situational phobias but less frequent fears of harm or injury.
A study of the literature suggests a wide range in prevalence that may be influenced by, among other things, age, intellectual capacity, level of functioning, and specific ASD diagnoses. There is a lack of a gold standard instrument to precisely capture anxiety symptoms in ASD. Even while the evolution of anxiety symptoms in neurotypical children is comparable, there are a few distinctions that need to be taken into consideration. For instance, ASD children may not express their anxieties or worries due to their inadequate insight, acting out behaviorally as an alternative.
Learn more about the link between anxiety and ASD.
Treatment options
Children with ASD and neurotypical children receive similar treatments for anxiety. There is some evidence to support the efficacy of modified cognitive behavioral therapy in high-functioning ASD, hence a multimodal approach is advised. There are few pharmacological studies on this population. To meet sensory and special education needs, behavioral interventions must also be taken into account.
Depression
Between 0.9 and 10% of people with ASD are found to have depression. Numerous studies have shown that higher levels of functioning, adaptation, self-awareness of one’s own limitations, and cognitive level of functioning are all strongly connected with lower incidences of depression.
However, the diagnosis and management of this problem would be improved by a high level of vigilance and regular screening. The diagnosis of depression is mostly based on the patient’s self-report of feelings and how those feelings affect everyday functioning. This information is frequently difficult to get in the community of people with ASD due to preexisting difficulties with verbal and social interaction.
In adolescents with Asperger syndrome, peer acceptance was found to be a predictor of depression, and worse friendship quality was associated with higher levels of anxiety and depression. Furthermore, depression was among the comorbid mental diseases that suggested antipsychotic therapy. The relationship between mood issues in ASD and emotional dysregulation, hypersensitivity, or an openly overwhelming response to daily stimuli has been hypothesized. Furthermore, depression is associated with being bullied, victimized in school, and experiencing family conflict.
Clinically speaking, it is still difficult to identify depression in people with ASD. The following ought to be taken into account in ASD, despite typical symptoms such as:
- Depressed mood
- Irritability
- Anhedonia
- Sleep or appetite disruptions
- Cognitive issues like impaired concentration
- Self-doubt
- A sense of hopelessness
- Distressing thoughts
- Somatic complaints
These include the following:
- Aggression
- Mood instability
- Hyperactivity
- Decreased self-care
- Reduced state of functioning
- Regression
- Variations in main symptoms
- Elevated compulsions
- Self-injurious behavior
- Catatonia
Treatment options
Although randomized controlled trials have not been sufficiently conducted to demonstrate the effectiveness of Selective Serotonin Reuptake Inhibitors SSRIs and Serotonin Norepinephrine Reuptake Inhibitors SNRIs in the treatment of depression and ASD, empirical findings support their usage as recommended in neurotypical children.
Mania
An unidentified predisposition for mood disorder comorbidity, without a distinct familial genetic component, is blamed for the 7% frequency of bipolar disorder with psychotic characteristics among people with Autism Spectrum Disorder ASD. However, some researchers that examined the family histories of autistic people discovered a high prevalence of serious affective illnesses, including bipolar disorder.
Mood issues in children with Autism and other difficulties may go unnoticed because the main indications of the disorder cover them up. The following may shift from baseline and be signs of mania:
- Obsessiveness
- Stereotypes
- Self-destructive behavior
- Hyperactivity
- Disturbed sleep
- As well as an increase in frivolity
- Distractibility
- Poor judgment
- Intrusiveness
- Excessive laughter
- Forced speech
- Agitation
Treatment options
Despite the fact that more thorough research is required, many medications, including atypical antipsychotics, lithium, and lamotrigine, have been empirically used to support the use of mood stabilizers in ASD. It has also been shown that divalproex sodium effectively reduces irritability, aggression, social connection, and mood swings.
Attention Deficit Hyperactivity Disorder
Attention Deficit Hyperactivity Disorder ADHD is characterized by symptoms of inattention, hyperactivity, and impulsivity in a variety of circumstances. The frequent co-occurrence of ADHD and ASD requires routine mutual assessment. ASD is thought to occur in 20 to 50% of children with ADHD. Whereas, ADHD is thought to occur in 30 to 80% of cases of ASD.
Optimizing behavioral and educational treatments is crucial. It may be required to do neuropsychological and psycho-educational testing in order to create an individualized educational plan.
Treatment options
In the setting of ASD, medication should be taken into consideration for the treatment of ADHD. Although response rates may be lower than in children with typical ADHD, methylphenidate is effective in lowering symptoms of inattention and hyperactivity in children with ASD. Furthermore, Risperidone with aripiprazole may be used to treat ADHD patients who exhibit aggression, agitation, or irritability or to address safety issues related to an elevated risk of accidents brought on by impulsivity.
Obsessive Compulsive Disorder OCD
Obsessive Compulsive Disorder OCD is characterized by recurring intrusive thoughts or images as well as repetitive behaviors. Despite the fact that diagnosis is typically made much later in life, the condition frequently begins in infancy and adolescence.
Studies suggest that there is a higher incidence of OCD in people with ASD and a higher rate of ASD among people who have also been diagnosed with OCD. According to family research, obsessive-compulsive traits in parents are linked to repetitive behaviors in autistic children. When considering rituals, repetitive behavior, and strict adherence to routines as basic characteristics of autism, the concurrent diagnosis can be debatable. The best indication that compulsion is related to OCD is when it is distressing and unwelcome (egodystonic), is preceded by thoughts that cause anxiety, and is used to alleviate anxiety. Rituals that are typical of autism are thought to be most likely to be satisfying and enjoyable for the child, actively engaged, egosyntonic, and not directly connected with earlier fear or subjective pain. Moreover, little insight which might be interpreted as knowledge of the irrationality of repetitious thoughts and behavior is anticipated in ASD.
Treatment options
Determining whether OCD is present in children with ASD is well worth the effort because the comorbidity may be amenable to particular treatments, like Cognitive Behavioral Therapy.
Catatonia
People with ASD may experience catatonic symptoms, which commonly begin in adolescence. Although catatonia in autism is uncommon. It is crucial to diagnose it because it can benefit from early intervention. And because severe instances run the risk of life-threatening complications. Because these diseases frequently exhibit echolalia, mutism, and stereotypical motions, diagnosing catatonia in ASD can be difficult.
The onset of catatonic symptoms in ASD may be slow, and in the early stages, they can manifest as a decline in self-care abilities, a loss of speech, and trouble starting tasks. Catatonia might be suspected when motor issues first appear such as the following:
- Becoming stuck mid-action
- Having trouble initiating movements
- Becoming immobile
- Increasing repeated behaviors
- Having trouble crossing thresholds
- Maintaining postures
If repetitive behaviors are congruent with a person’s standard ASD symptoms, such as stereotypic motions and echolalia, they should not be included in the diagnosis of catatonia.
We hope you found this article helpful in learning more about common comorbid psychiatric disorders in Autism. Learn more about the Types Of Behavioral Therapy For Autism Spectrum Disorders
Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, et al. (2008) Psychiatric disorders in children with Autism Spectrum Disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry 47:921-929.
Romero, M., Aguilar, J. M., Del-Rey-Mejías, Á., Mayoral, F., Rapado, M., Peciña, M., Barbancho, M. Á., Ruiz-Veguilla, M., & Lara, J. P. (2016). Psychiatric comorbidities in Autism Spectrum Disorder: A comparative study between DSM-IV-TR and DSM-5 diagnosis. International Journal of Clinical and Health Psychology : IJCHP, 16(3), 266-275. https://doi.org/10.1016/j.ijchp.2016.03.001
Kirsch AC, Huebner ARS, Mehta SQ, et al. Association of Comorbid Mood and Anxiety Disorders With Autism Spectrum Disorder. JAMA Pediatr. 2020;174(1):63–70. doi:10.1001/jamapediatrics.2019.4368



 Healing Your Inner Child: A Short Guide
Healing Your Inner Child: A Short Guide  What You Need to Know About Trauma & its effects
What You Need to Know About Trauma & its effects  Dealing with a Narcissistic Parent: Strategies and Support
Dealing with a Narcissistic Parent: Strategies and Support  Understanding the MBTI Personality Types
Understanding the MBTI Personality Types  Understanding the Big Five Personality Traits
Understanding the Big Five Personality Traits  Body Image: what it entails and how it affects you
Body Image: what it entails and how it affects you